What is Discectomy Surgery?
Discectomy is a surgical procedure performed on the lower
back (lumbar region) to remove part or all of a herniated disc that is exerting
pressure on the spinal cord or nerves. By removing the affected portion of the
disc, the surgery helps alleviate numbness, weakness, and pain associated with
nerve compression.
Who Needs Discectomy Surgery?
Discectomy is recommended for patients experiencing:
Persistent lower back pain that radiates to the legs- Numbness
or tingling sensations due to nerve compression
- Muscle
weakness in the legs
- Lack
of improvement with conservative treatments like physiotherapy or medications
Discectomy is typically performed by a Neurosurgeon
or Orthopedic Spine Surgeon who specializes in spinal disorders and
surgeries.
What Happens Before Discectomy Surgery?
Prior to surgery, the patient undergoes:
- Medical
Evaluation: A thorough assessment including MRI or CT scans to
determine the severity of the herniated disc.
- Preoperative
Tests: Blood tests, ECG, and other necessary evaluations to assess
overall health.
- Consultation
with the Surgeon: The doctor explains the procedure, risks, and
expected recovery.
- Lifestyle
Adjustments: Patients may be advised to stop certain medications and
avoid smoking/alcohol before surgery.
Once you have completed your Pre-surgery paperwork, an
anesthesiologist will start an IV (an intravenous line) that will be used to
administer medications and fluids during your surgery. The complete
procedure consists of five steps and takes approximately two hours.
1. Prepping you for surgery:
- Once
you are resting comfortably on the operating table you will be given
anesthesia.
- When
you are asleep you will be placed onto your stomach, your sides and chest
will be supported with pillows.
- The
area where the incision will be made will be cleaned and prepared for the
surgery.
2. The incision:
- A
fluoroscope (a special type of X-ray) will be used to guide your surgeon.
- A
thin needle will be placed through the skin to the bone to find the
damaged disc and vertebra.
- Open
Discectomy:
- The
physician will make an incision in your back over the targeted vertebrae.
- The
incision will be approximately one to two inches long. Longer
incisions will be needed if more than one vertebrae is affected.
- The
muscles are moved aside to reveal the vertebra below.
- An
X-ray will be used to confirm which vertebra needs to be operated on.
- Minimally
invasive Discectomy:
- An
incision of one inch or less is made on one side of the back.
- Dilators
are used to separate the muscles and gain access to the vertebra.
3. Laminotomy:
A very small opening will be made in the lamina (the
vertebral arch), the flat plates of bone that protect the spinal cord, by
removing the bone above and below the vertebrae. The spinal cord and
nerves are gently moved aside to access the herniated disc.
4. Disc fragment removal:
- The
nerve root protective sac is gently moved aside.
- A
surgical microscope is used to identify the herniated disc.
- The
surgeon removes the ruptured section of the disc that is compressing the
nerve.
- Any
bone spurs that are discovered are also removed.
- If
fusion is needed to treat instability of the spine it will be performed at
this time.
5. Closure:
- The
equipment holding the muscles apart is removed.
- The
muscle is stitched or stapled together.
- The
skin is stitched or stapled together.
- A
sterile dressing is placed over the incision to keep it clean.
Discectomy: Cost and Procedure in India
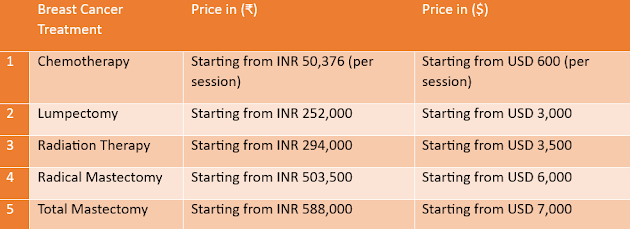
The average cost of Discectomy Surgery in India starts from INR
294,000 ($3,500). However, the final cost may vary depending on several
factors, including the severity of the condition, the surgeon's expertise, and
the type of hospital chosen.
- Hospital
Stay: Patients may stay in the hospital for 1-2 days.
- Pain
Management: Medications are prescribed to manage post-surgical pain.
- Physical
Therapy: Patients are encouraged to start light movements and
gradually resume normal activities.
- Recovery
Timeline: Most patients recover within 4-6 weeks, but full
recovery may take up to three months.
Q1: Is Discectomy Surgery safe? Yes, it is a common
and safe procedure when performed by an experienced surgeon.
Q2: How long is the recovery period? Most patients
resume daily activities within 4-6 weeks.
Q3: Are there any risks involved? As with any
surgery, risks include infection, bleeding, or nerve injury, but they are rare.
Q4: Will I need physiotherapy after surgery? Yes,
physical therapy helps in faster recovery and strengthening the spine.
Q5: Can a herniated disc reoccur after surgery? While
the chances are low, it is possible if preventive measures are not followed.
Conclusion
Discectomy surgery in India is a cost-effective solution for
individuals suffering from herniated disc-related issues. With advanced medical
infrastructure, skilled surgeons, and affordable treatment options, India has
become a preferred destination for spinal surgeries. If you are considering
Discectomy, consult a spine specialist to determine the best course of action
for your condition.